Due to population growth and economic development, our planet is experiencing significant changes in natural ecosystems that may lead to the re-emergence of infectious diseases. For 5 years, ECOMORE 2 project, coordinated by Institut Pasteur in partnership with the Institut Pasteur du Cambodge, the Institut Pasteur du Laos, the National Health Laboratory (NHL) of Myanmar, the Research Institute for Tropical Medicine (RITM) in the Philippines and National Institute of Hygiene and Epidemiology (NIHE) in Vietnam, have led epidemiological and entomological studies to understand the impact of climate change on water-and-vector-borne diseases such as dengue and leptospirosis.
Southeast Asia faces significant climate change threats, with increasing typhoons, floods, and monsoons. Rising water levels contribute to the spread of disease-carrying mosquitoes such as dengue. The AFD-funded ECOMORE 2 project aimed to better understand the ecological mechanisms, threat and risk factors to the local population for the emergence of infectious diseases. Through close national and regional collaborations, the project worked to strengthen surveillance systems and provide recommendations for effective public health interventions, facilitating the implementation of appropriate measures.
Dengue, a priority disease for health authorities in Southeast Asia
According to the World Health Organization, dengue is the most widespread and rapidly increasing vector-borne disease.1.3 billion people live in dengue endemic areas in 10 countries of Southeast Asia. As part of the ECOMORE 2 project, national health authorities of Cambodia, Philippines, and Lao PDR prioritized dengue to assess if a control program could reduce human transmission and alleviate hospital overcrowding during the epidemic season.
In Lipa City, Philippines, known to be a dengue hotspot during outbreaks, the RITM conducted a parallel two-armed cluster randomized trial to evaluate the effectiveness of In2Care® mosquito traps in reducing Aedes aegypti mosquito populations and preventing dengue transmission in children aged 6-16. The study included 46 clusters, each with 50 to 100 children, divided into two groups: 23 clusters with the intervention (In2Care® traps) and 23 clusters as the control. At the same time, saliva samples were collected from the children on three occasions over 5 months to assess virus exposure. While the traps did not reduce mosquito density possibly due to the potential cleaning of the traps by households, the study found a notable reduction in the occurrence of dengue seroconversion in children.
In Cambodia, the Institut Pasteur du Cambodge chose to target schools in peri-urban areas. An integrated vector control approach was implemented involving breeding site destruction, larvicide, the In2Care® traps, and informing students and teachers of dengue and its vectors. Active monitoring of dengue-like syndrome and serological monitoring was also conducted in collaboration with health centers.
Four years of monitoring showed that schools are not hotspots for dengue transmission (probably due to the limited time spent at schools) but living near the Mekong River and being between the age of 5 and 10 greatly increases the risk of developing dengue-like illness and dengue fever. Institut Pasteur du Cambodge’s entomological and anthropological teams raised awareness on the role of plastic waste as breeding sites for vectors, the importance of removing it and installing closed taps or cisterns. However, virologists concluded that these interventions alone did not reduce dengue transmission. Thus, a community-based approach should be considered in the future to curb dengue incidence.
Additionally, in Lao PDR, vector dynamics was investigated by Institut Pasteur du Laos in urban areas using auto-dissemination traps, showing that these did not reduce the risk of dengue contamination, likely due to insufficient destruction of breeding sites. Yet, a weekly entomological inventory confirmed Aedes activity in the dry season supporting the recommendation for effective vector control measures in this period.
Cambodia and Lao PDR have the same dengue serotypes as China, which can be attributed to heavy traffic from infrastructure development. A disease data management system and epidemic simulator were developed to help national and regional health authorities make efficient decisions during epidemic peaks. Entomological studies in both countries showed the effectiveness of various control strategies for Aedes mosquitoes, including traps, larvicides, and communication with the population. These measures led to a decrease of Aedes larvae and a reduction of female Aedes aegypti mosquitoes. The study revealed their resistance to some commonly used insecticides, prompting authorities to replace certain insecticides to more efficient ones.
Is climate change amplifying the burden of the disease?
Health geographers from the Institut de Recherche pour le Development (IRD) used weather and landscape analysis to study the correlation of the distribution and diversity of mosquitoes and environmental factors. It was observed that the local disparity in the distribution of these vectors seemed to be more influenced by the environment than by weather. New modelling techniques based on satellite observation, were used to study mosquito species and gather environmental data. The operated meteorological models developed patterns for the presence, seasonality and dynamics of Aedes aegypti and Aedes albopictus, both dengue fever vectors.
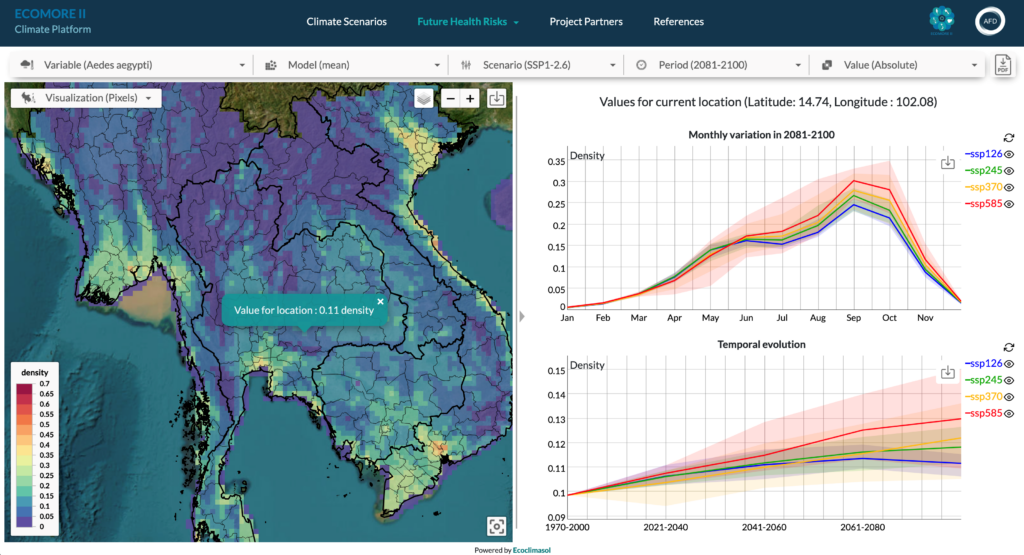
The models were integrated into a user-friendly climate platform to assess the impact of prospective climate scenarios on their future distribution. For instance, studying the disease’s spread during rainy episodes enabled the creation of detailed long-term models spanning several decades.
Results show that by the end of the century, Ae. aegypti and Ae. albopictus densities will increase by up to 46% and 25%, respectively, in Southeast Asia due to rising temperature. Climate mitigation measures are unlikely to significantly moderate this expansion.
To enhance disease risk prediction amidst climate change, a crucial third phase of the ECOMORE project is proposed. One focus could be to study the impact of climate and environmental changes on the spatial-temporal distribution and circulation of pathogens of public health interest, considering humans, animals, and vectors to release recommendations to national authorities and policy makers for appropriate public health interventions.
*******************************************
What is dengue ?
Dengue belongs to the Flaviviridae family, like West Nile virus and yellow fever virus. Considered as a re-emerging disease, it is transmitted to humans by Aedes aegypti & Aedes albopictus mosquitoes. The dengue virus strains are classified into four different serotypes: DENV-1, DENV-2, DENV-3 and DENV-4. Acquired immunity because of infection by one serotype provides protection against that particular serotype, but not against the others. Subsequent infection by another serotype potentially increases the risk of severe dengue, which has been more and more widely reported during recent outbreaks.